Georgetown health officials report syringe-service program outcomes; cite disease detection, referrals and treatment linkages
Get AI-powered insights, summaries, and transcripts
Subscribe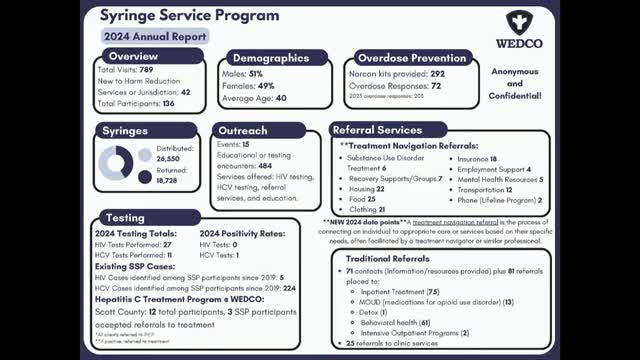
Summary
Dr. Miller presented the syringe-service program’s annual report at a joint Georgetown-Scott County workshop, citing disease detection, naloxone distribution, overdose responses and referrals for treatment and social services.
At a joint workshop for Georgetown City Council and Scott County fiscal court, Dr. Miller of the local health department presented the annual report for the county’s syringe-service program and described how the program has expanded into broader harm-reduction and referral services.
Dr. Miller said the program began in February 2019 and that the 2024 annual totals show 789 total visits (not unique people), 42 clients new to harm reduction and 136 active participants in the program. She reported an average participant age of about 40.
The program, Dr. Miller said, has distributed 292 naloxone (Narcan) kits and documented 72 overdose responses tracked in coordination with EMS through an overdose-mapping system (ODMAP). Outreach events numbered 15 during the reporting period, with 484 related encounters. The health department reported 6 referrals to substance use disorder treatment, 7 referrals to recovery support groups, 22 housing referrals, 25 food referrals and additional referrals for clothing, insurance enrollment and employment assistance; the program’s staff are trained to enroll clients in insurance on site.
“These are touch points,” Dr. Miller said, describing the program’s purpose as disease detection and connection to services. She reported that since program inception the clinic has identified five HIV cases and 224 hepatitis C cases, and that a nurse practitioner on staff can initiate hepatitis C treatment in-house. Dr. Miller said 12 participants had accepted referrals into hepatitis C treatment; she estimated that treating those cases could avoid roughly $1 million in future medical costs if treatment is completed.
Dr. Miller described operational details requested by local leaders: the program uses retractable syringes to reduce public safety risk and operates from the health department, consistent with the authorization noted in local briefing materials. She said the program partners with the University of Kentucky (which provides a staff member for the project), EMS, the Angel program, Gathering Place Mission, Amen House, Isaiah House and local recovery providers.
Council members and other officials asked about youth outreach, vaping education in schools and barriers to treatment. Dr. Miller said the work is anonymous and confidential and that each participant is tracked with a unique identifier rather than by name. She also noted that the local syringe-service staff trained on the state referral network (Connect) to coordinate wraparound services.
Officials asked whether opioid-abatement funds could support the program; Dr. Miller said those funds have been tightly specified in the past and that the health department’s personnel costs are primarily supported by a University of Kentucky staff placement.
The workshop did not include votes on the program; council and fiscal court members thanked staff for the report and discussed continuing community supports and referrals, including ongoing jail treatment pilot work and partnerships with Isaiah House and Recovery Works.
