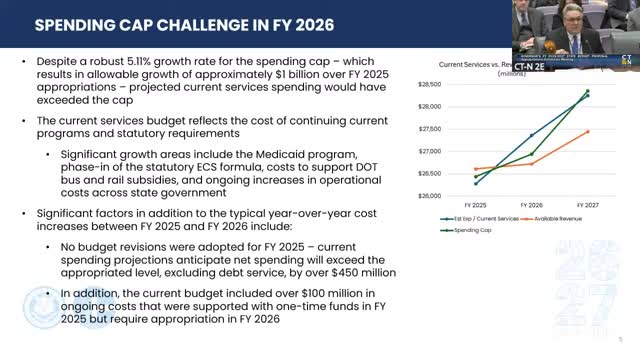
Administration cites $300M Medicaid deficiency; proposes targeted coverage and rate changes
Summary
OPM told lawmakers a roughly $300 million Medicaid shortfall is driving much of the first-year budget constraint and described several proposed savings: removing some weight-loss drug coverage, rolling back ambulance rates, freezing an eligibility program, and targeted rate increases in later years.
Jeff, secretary of the Office of Policy and Management, told the committee that Medicaid growth and related current-services costs consumed nearly all available cap growth in fiscal 2026 and that the administration is projecting "about $300,000,000 over the enacted budget just for the Medicaid program alone."
To reduce projected spending, the administration proposed several changes to Medicaid and related programs. Those changes include removing coverage for certain weight-loss drugs when prescribed solely for weight loss while continuing coverage when prescribed for diabetes or to reduce cardiac-event risk; a rollback of ambulance rates to fiscal 2024 levels; a freeze in eligibility thresholds for the Medicaid program for employees with disabilities at their April 2025 levels; and a proposal to require pharmacies to dispense a 30-day supply in most cases to reduce dispensing fees. The presentation said the package yields $28.8 million in savings in fiscal 2026 and about $16.9 million in fiscal 2027 for the weight-loss-drug change alone, and additional savings from the other measures.
At the same time, the governor's budget proposes targeted rate increases: the administration recommended funding that would translate to roughly $21 million for rate increases in fiscal 2026 and more than $50 million in fiscal 2027 as part of a targeted rate-setting process aligned with a recent Medicaid rate study. The presentation said those increases would be tied to access and quality goals and intended to reduce acute-care spending over time.
Why it matters: Committee members pressed the administration on whether eliminating coverage would increase long-term health costs. Senator Kushner and Representative Nutrio asked whether the proposed removal of weight-loss-drug coverage had been assessed for downstream cost impacts; the secretary said such decisions were meant to keep the budget under the statutory cap and that some private carriers and other states are rethinking coverage because of rapid cost growth.
Context and limits: The administration described some of these as difficult but necessary choices to keep the biennial budget under the cap. The presentation acknowledged the changes would require statutory and administrative steps where applicable. Lawmakers repeatedly asked for more analysis on the long-term clinical and fiscal effects of the proposed changes.