Senate bill would bar vision plans from cutting provider pay below 95% of Medicaid rate, sponsors say
Get AI-powered insights, summaries, and transcripts
Subscribe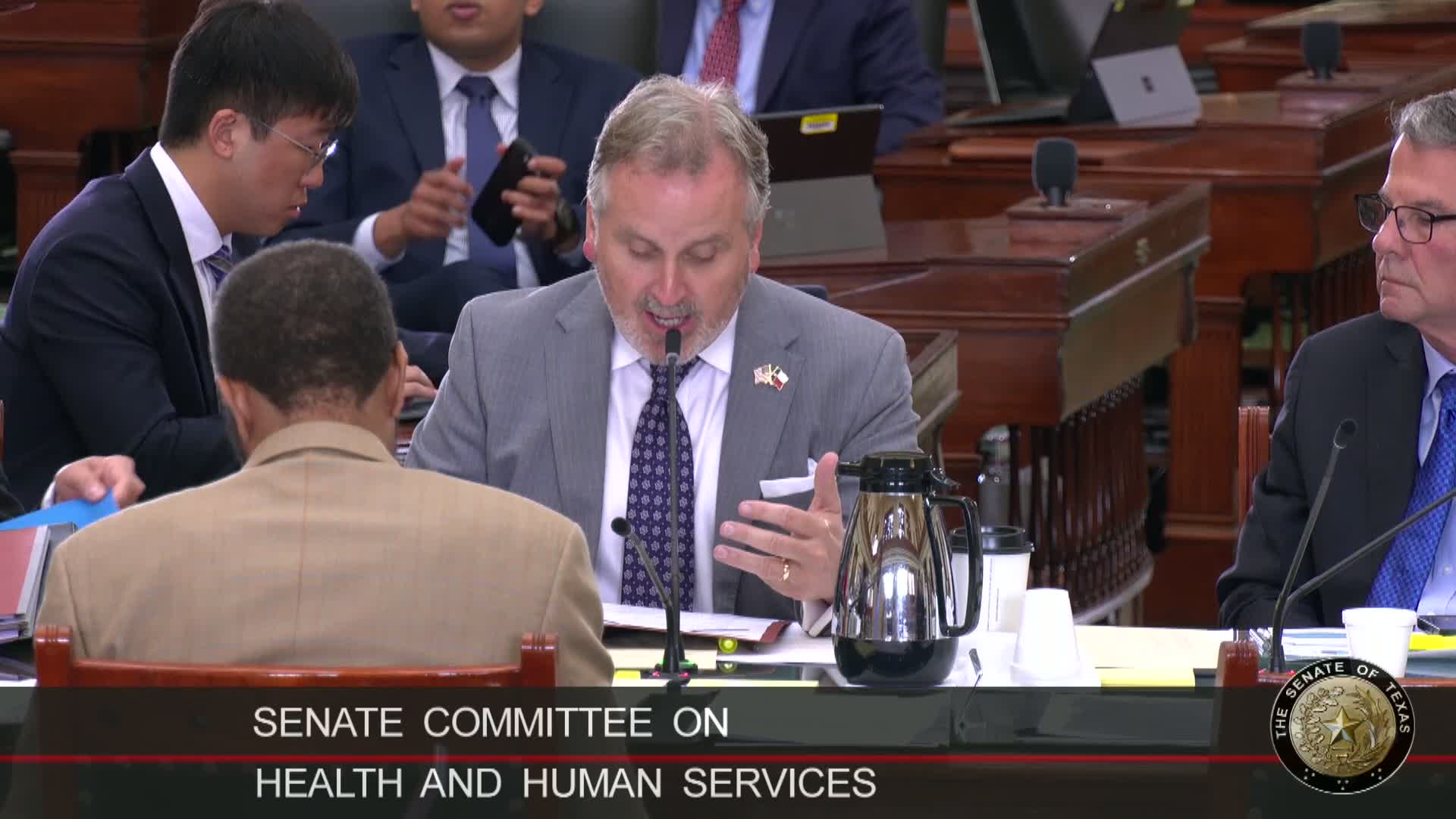
Summary
Senate Bill 2450 would prohibit vision‑plan subcontractors to Medicaid MCOs from cutting optometrist pay below 95% of the state‑determined Medicaid rate; optometrists testified the practice has led to unsustainably low reimbursements.
Senate Bill 2450, carried by Sen. Hughes, would set a minimum reimbursement floor when Medicaid managed‑care organizations subcontract vision benefits to third‑party vision plans. The committee substitute narrows the original measure to address reimbursement and removes a fiscal note from the bill text.
Sponsor’s presentation and problem described: Sen. Hughes said optometrists across Texas report vision‑plan fee schedules that are far below state Medicaid rates when MCOs subcontract to vision plan companies. He said the state‑determined Medicaid rate for a basic eye exam is $71.29 while some vision plans reimburse as little as $30—an estimated 58% reduction—leaving providers unable to cover the cost of services and at risk of leaving Medicaid altogether.
Provider testimony: Optometrists who testified said MCOs sometimes require providers to contract with vision‑plan subcontractors that then impose nonnegotiable, deeply reduced fee schedules. Dr. Tommy Lucas (Killeen) and Dr. Mary Kate Walters (Brenham) told the committee the 95% floor in the committee substitute is a workable compromise that will keep providers in the system while allowing MCOs some administrative flexibility.
Health‑plan perspective: Jamie Dudensing of the Texas Association of Health Plans urged caution, noting that managed care’s flexibility to negotiate private market rates is a core element of the managed‑care model. Dudensing said the state typically does not set statutory rate floors for Medicaid managed‑care reimbursements and that MCOs administer risk and negotiate rates to keep the program affordable.
Committee action: The committee heard invited and public testimony and left the bill pending. Sponsor and providers said the measure aims to preserve provider participation in Medicaid networks and prevent urban‑rural disparities in access to eye care.
