Senate approves surprise-billing bill for out‑of‑network ambulance services; sets Jan. 1, 2026 effective date
Get AI-powered insights, summaries, and transcripts
Subscribe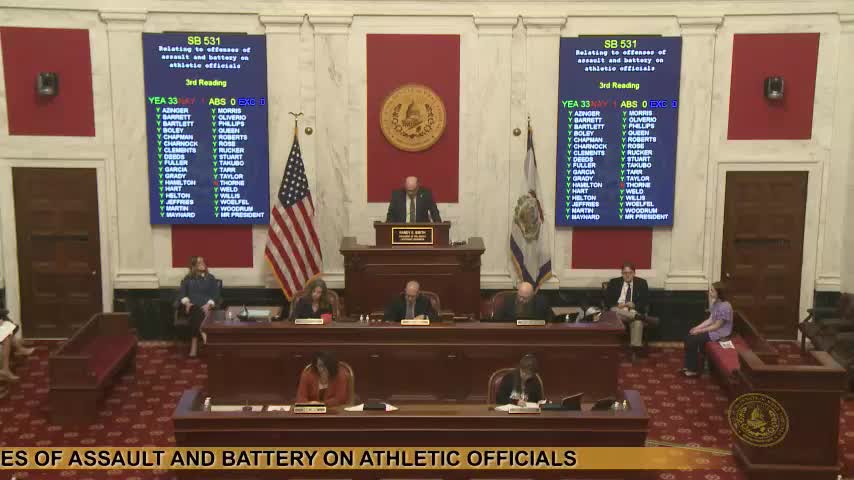
Summary
Senate Bill 632, which bars surprise billing by out‑of‑network ambulance providers and establishes prompt insurer payment rules, passed unanimously and was later scheduled to take effect Jan. 1, 2026.
The West Virginia Senate unanimously approved Committee Substitute for Senate Bill 632 on third reading, a measure aimed at preventing surprise bills from out‑of‑network ambulance providers and setting rules for timely insurer payment.
On the floor the senator from Ohio said the bill “prohibit[s] surprise billing by emergency medical service agencies” and requires insurers to remit payment to an out-of-network agency within 30 days of receiving a clean claim in most situations. The sponsor also said the bill requires written explanation if an insurer denies a claim.
The Senate passed the bill on a recorded vote of 34 yays, 0 nays. The senator from Lewis then moved to make the bill effective Jan. 1, 2026; that motion was approved on the floor by the required two‑thirds vote and the clerk declared the bill effective 01/01/2026.
Why it matters: The passage targets a common source of consumer surprise bills in emergency medical transport and formalizes timelines for insurer payments and claimant notices. The effective date gives insurers and provider networks time to adjust to claims‑payment procedures.
Next steps: The clerk will communicate the action to the House and the bill will proceed toward enrollment and signature as provided under legislative rules.
