Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.
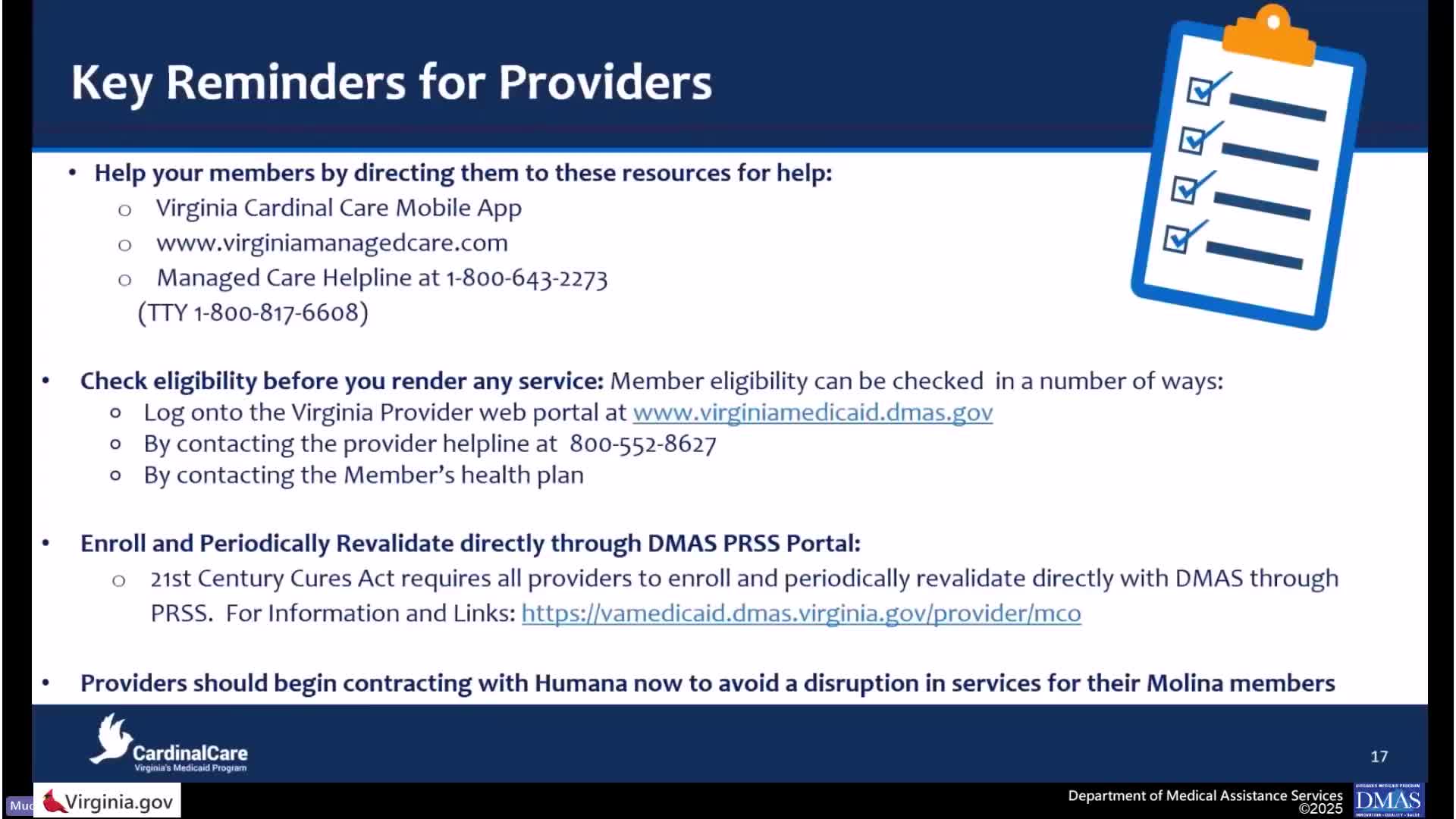
Providers told how to enroll, credential and contract for CCMC; plans list claims timing, remittance tools and training
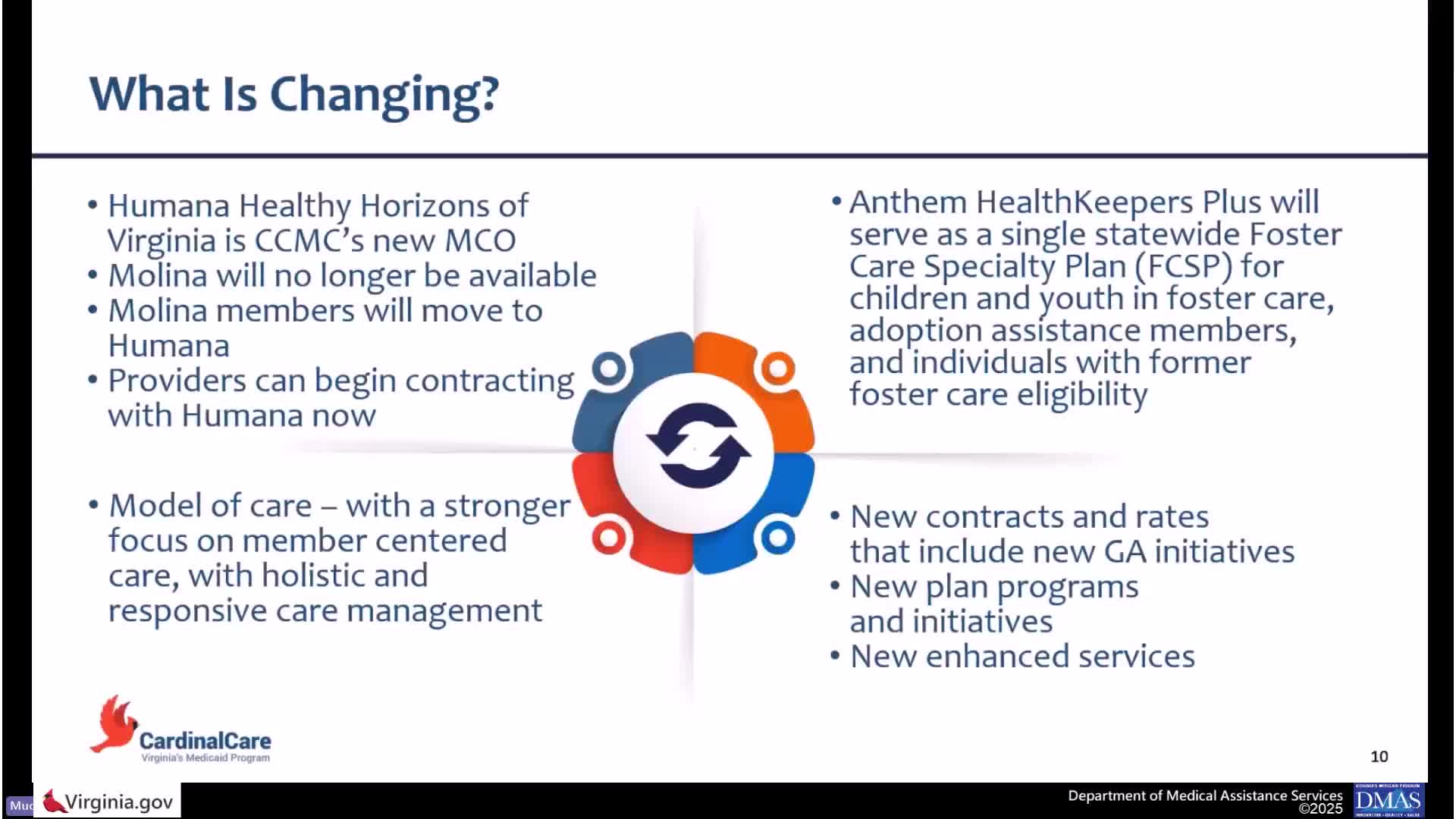
Molina members move to Humana Healthy Horizons July 1; plans, DMAS say prior authorizations and waivers honored during transition