Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.
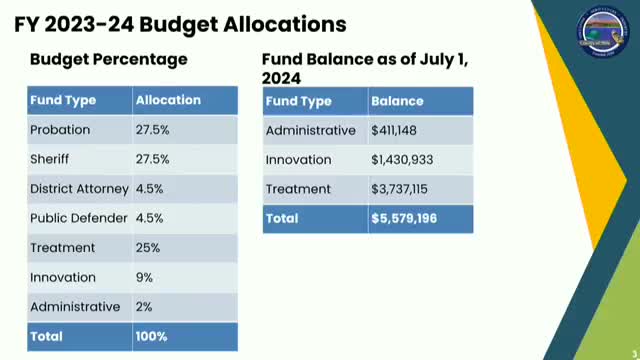
Yolo County Community Corrections Partnership reports $5.5 million fund balance, outlines programs and day‑reporting work

Board directs staff to apply for state grant to support Prop 36 implementation

Yolo County officials warn of $11 million MHSA shortfall as state shifts to Behavioral Health Services Act

First 5 Yolo outlines Welcome Baby/Road to Resilience expansion and shift to external funding

Sacramento‑Yolo Mosquito & Vector Control warns of West Nile season, outlines new sterile‑male trial