Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.

Montana hearing on House Bill 783: sponsors and medical groups urge insurer coverage for GLP‑1 weight‑loss drugs; insurers warn of large fiscal impact
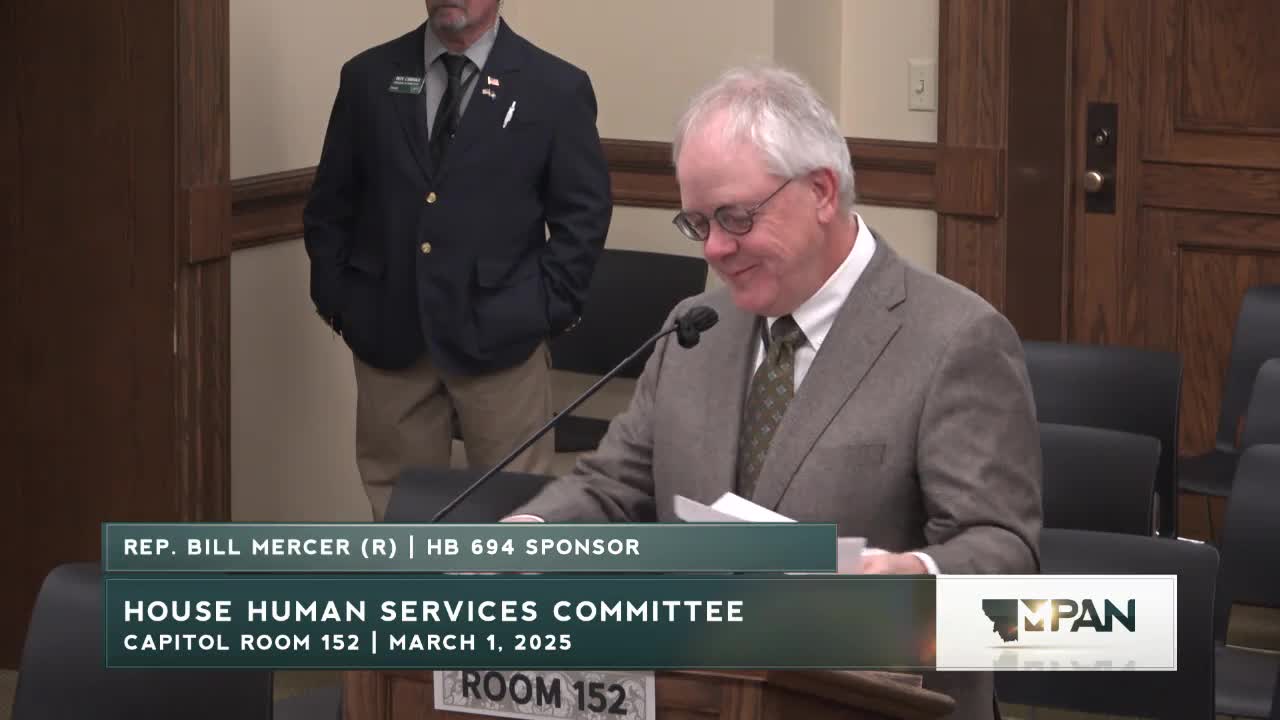
Bill restores statute text governing emergency‑use vaccines after district court ruling; sponsor says it simply re‑places prior language
Bill would let patients verbally name a ‘trusted decision maker’ in medical chart when they still have capacity

Committee clears bill to confirm licensing boards can obtain health records under subpoena consistent with HIPAA
Montana bill would reestablish guardianship stakeholder group (WINGS) to recommend reforms; AARP and advocates back reinstatement