Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.

Officials flag rising specialty drug costs, rebates and accelerated‑approval risks in Medicaid pharmacy briefing
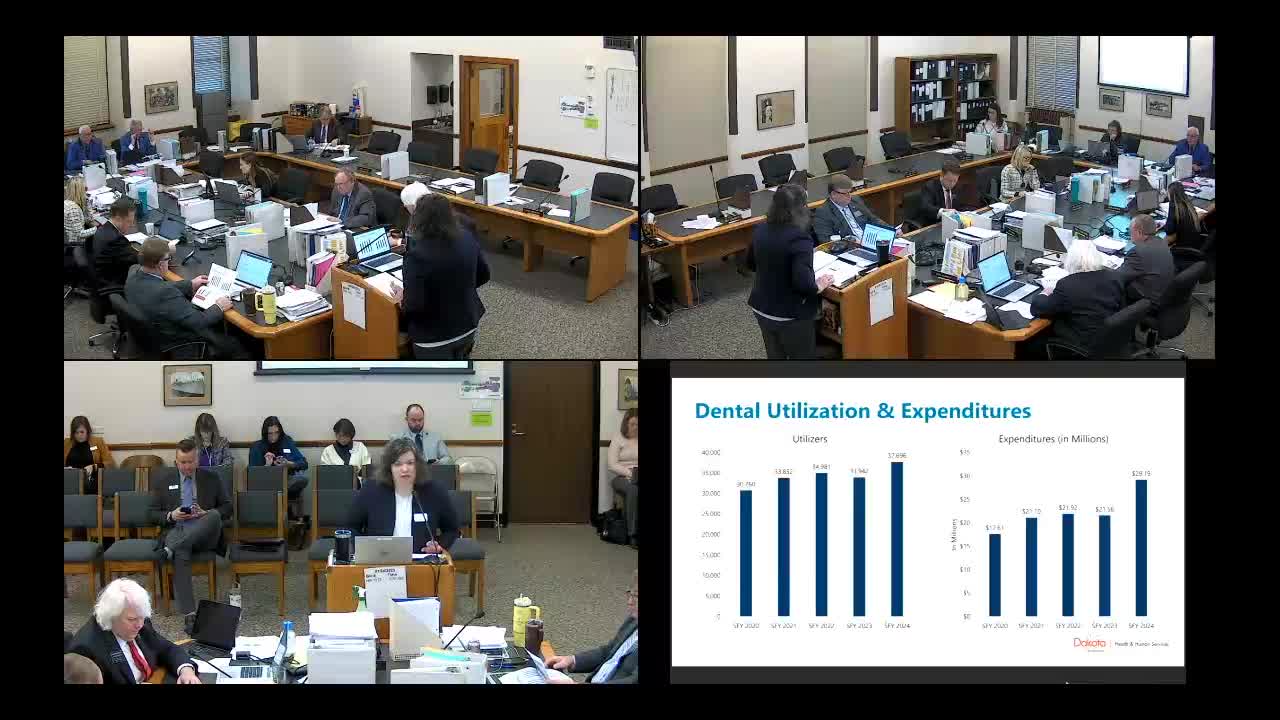
Lawmakers hear low performance on children's dental access; rebasing not in governor’s budget